 Wirral Surgeon
Excellence for Life
Wirral Surgeon
Excellence for Life
Procedures
The most important point to remember is that everyone with a bowel problem can be helped and many can be completely cured.
Whenever possible, we offer procedures using minimally invasive techniques.
Fistula Surgery
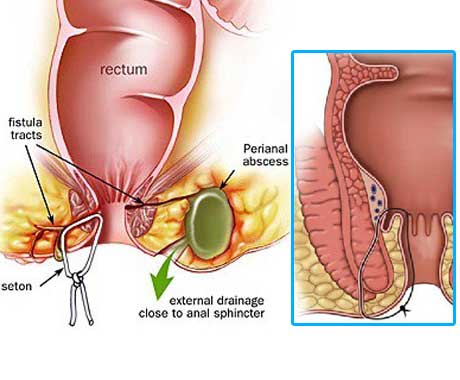
Treatment of fistula-in-ano remains challenging. No definitive medical therapy is available for this condition, though long-term antibiotic prophylaxis and infliximab may have a role in recurrent fistulas in patients with Crohn disease. Surgery is the treatment of choice, with the goals of draining infection, eradicating the fistulous tract, and avoiding persistent or recurrent disease while preserving anal sphincter function.
Therapeutic intervention is indicated for symptomatic patients. If patients are without symptoms and a fistula is found during a routine examination, no therapy is required.
Fistula Surgery
Treatment of fistula-in-ano remains challenging. No definitive medical therapy is available for this condition, though long-term antibiotic prophylaxis and infliximab may have a role in recurrent fistulas in patients with Crohn disease. Surgery is the treatment of choice, with the goals of draining infection, eradicating the fistulous tract, and avoiding persistent or recurrent disease while preserving anal sphincter function.
Therapeutic intervention is indicated for symptomatic patients. If patients are without symptoms and a fistula is found during a routine examination, no therapy is required.
Workup
Rectal irrigation with enemas should be performed on the morning of the operation. Anesthesia can be general or by using a regional block. Preoperative antibiotics are usually administered.
Fistulotomy
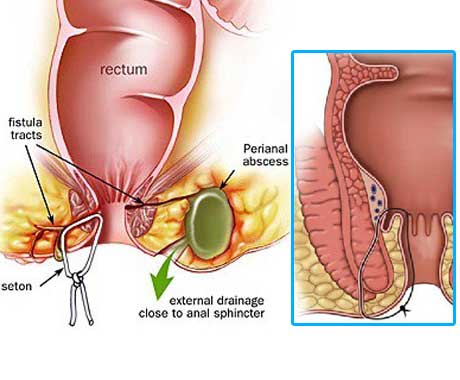
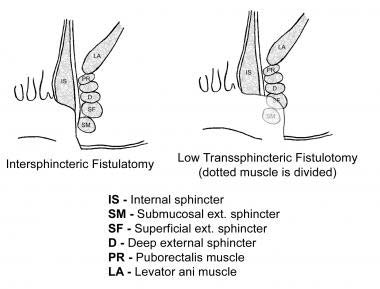
The laying-open technique (fistulotomy) is useful for 85-95% of primary fistulas (ie, submucosal, inter-sphincteric, and low trans-sphincteric; see the image).
A probe is passed into the tract through the external and internal openings. The overlying skin, subcutaneous tissue, and internal sphincter muscle are divided with a knife or electrocautery, and the entire fibrous tract is thereby opened. Curettage is performed to remove granulation tissue in the tract base.
Complete fistulectomy creates larger wounds that take longer to heal and offers no recurrence advantage over fistulotomy.
Single-Stage Seton (cutting)
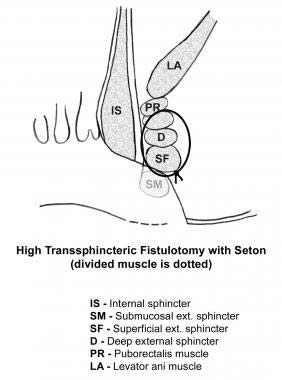
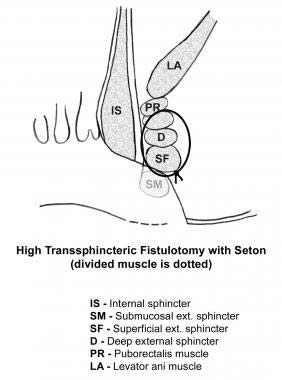
A thread (seton) is passed through the fistula tract around the deep external sphincter after opening the skin, subcutaneous tissue, internal sphincter muscle, and subcutaneous external sphincter muscle. The seton is tightened down and secured with a separate silk tie.
With time, scarring occurs above the seton as it gradually cuts through the sphincter muscles. The seton is tightened on subsequent office visits until it is pulled through over 6-8 weeks. A cutting seton can also be used without associated fistulotomy.
Recurrence and incontinence are important factors to consider when this technique is employed. The success rates for cutting setons range from 82-100%; however, long-term incontinence rates can exceed 30%.
A thread (seton) is passed through the fistula tract around the deep external sphincter after opening the skin, subcutaneous tissue, internal sphincter muscle, and subcutaneous external sphincter muscle. The seton is tightened down and secured with a separate silk tie.
With time, scarring occurs above the seton as it gradually cuts through the sphincter muscles. The seton is tightened on subsequent office visits until it is pulled through over 6-8 weeks. A cutting seton can also be used without associated fistulotomy.
Recurrence and incontinence are important factors to consider when this technique is employed. The success rates for cutting setons range from 82-100%; however, long-term incontinence rates can exceed 30%.
Two-stage seton (draining/fibrosing)
Unlike the cutting seton, the seton is left loose to drain the intersphincteric space and to promote fibrosis in the deep sphincter muscle. Once the superficial wound is healed completely (2-3 months later), the seton-bound sphincter muscle is divided.
Mucosal Advancement Flap
A mucosal advancement flap is reserved for use in patients with chronic high fistula but is indicated for the same disease process as seton use. Advantages include a one-stage procedure with no additional sphincter damage. A disadvantage is poor success in patients with Crohn disease or acute infection.
This procedure involves total fistulectomy, with removal of the primary and secondary tracts and complete excision of the internal opening.
Fibrin glue and fistula plugs (Surgisis)
These procedures have a less-invasive nature, associated with decreased postoperative morbidity and risk of incontinence; however, long-term data are lacking for eradication of disease, especially in complex fistulas, which carry high recurrence rates.
LIFT Procedure
Ligation of the intersphincteric fistula tract (LIFT) is a sphincter-sparing procedure for complex transsphincteric fistulas. It is performed by accessing the intersphincteric plane with the goal of performing a secure closure of the internal opening and by removing the infected cryptoglandular tissue. The curettaged wound is left open.
Diversion
In rare cases, the creation of a diverting stoma may be indicated to facilitate the treatment of a complex persistent fistula-in-ano. The most common indications include patients with perineal necrotizing fasciitis, severe anorectal Crohn’s disease and radiation-induced fistulas.
Complications
Early postoperative complications may include the following:
Delayed postoperative complications may include the following:
Postoperative rates of recurrence and incontinence vary according to the procedure performed: