 Wirral Surgeon
Excellence for Life
Wirral Surgeon
Excellence for Life
Condition treated
The most important point to remember is that everyone with a bowel problem can be helped and many can be completely cured.
It is never too late to get help with your bowel problems. If you would like some advice on how to approach your GP regarding your bowel problem do get in touch.
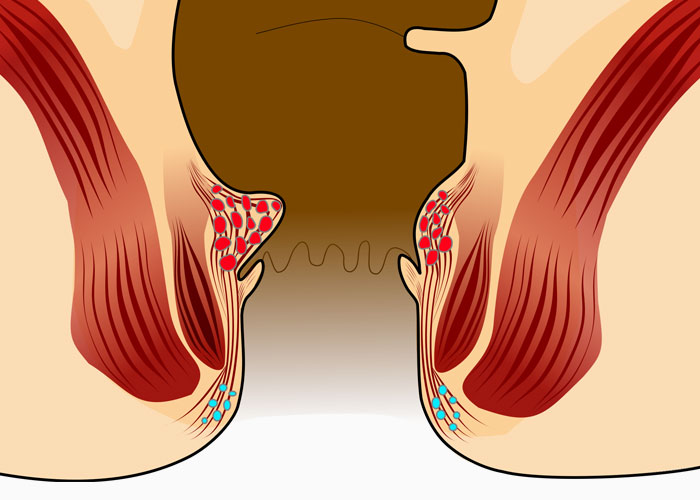
About Haemorrhoids
Haemorrhoids are venous cushions (blood vessels) of the ano-rectum and are universally present unless a previous intervention has taken place. Although haemorrhoids are a common condition, many patients are too embarrassed to ever seek treatment. Worldwide, the prevalence of symptomatic haemorrhoids is estimated at 4.4% in the general population. The prevalence of haemorrhoids increases with age, with a peak in persons aged 45-65 years.
Clinical presentation
The most common symptoms of haemorrhoids are rectal bleeding, pain, itching (pruritus), or prolapse. Rectal bleeding is the most common problem. The blood is usually bright red and may drip, squirt into the toilet bowl, or appear as streaks on the toilet paper. Pain truly caused by haemorrhoids usually arises only with acute thrombus (clot) formation. This pain peaks at 48-72 hours and begins to decline by the fourth day.
The presence/absence of prolapse allows grading of haemorrhoids:
Differential diagnosis
Other conditions that should be considered when evaluating a patient with suspected haemorrhoids include:
Management
Haemorrhoids should only be treated when causing significant symptoms; no matter how bad the haemorrhoids look to the practitioner, they should not be treated unless they bother the patient. The following is a quick summary of treatment for internal haemorrhoids by grade:

Thrombosed external haemorrhoids are treated surgically by removal of the clot if the patient presents early (typically within 72 hours from the onset of pain); conservative measures are recommended for late presentations.