 Wirral Surgeon
Excellence for Life
Wirral Surgeon
Excellence for Life
Procedures
The most important point to remember is that everyone with a bowel problem can be helped and many can be completely cured.
Whenever possible, we offer procedures using minimally invasive techniques.
Haemorrhoid Procedures
Sometimes piles can be treated by making a few changes to your diet and lifestyle. The aim is to help relieve your symptoms. There are a number of things that you can do to help.
Surgical treatments for piles are an option if you have severe piles, other treatments haven’t worked, or your piles keep bleeding.
Haemorrhoid Procedures
Sometimes piles can be treated by making a few changes to your diet and lifestyle. The aim is to help relieve your symptoms. There are a number of things that you can do to help.
Surgical treatments for piles are an option if you have severe piles, other treatments haven’t worked, or your piles keep bleeding.
Conservative management
Medical management is the initial treatment of choice for grade I internal and non-thrombosed external haemorrhoids. It consists of:
Many patients see improvement or complete resolution of their symptoms with conservative measures. More aggressive therapy is reserved for patients who have persistent symptoms after 1 month of conservative treatment.
Non-surgical procedures
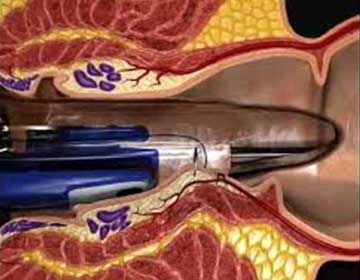
Rubber band ligation
Rubber band ligation is the most-used remedy for grade II and grade III hemorrhoids. Although rubber band ligation is effective in 75% of patients in the short term, it does not treat prolapsed hemorrhoids or those with a significant external component.
No anesthesia is required; complications are uncommon and usually benign. Necrotizing pelvic sepsis is a rare, but serious, complication of rubber band ligation. The diagnosis is suggested by the triad of severe pain, fever, and urinary retention. It occurs 1-2 weeks after ligation and requires prompt surgical debridement.
Infrared coagulation
Infrared coagulation works for grade I and II and some grade III hemorrhoids. This method may be as effective as banding with fewer and less severe complications.
Sclerotherapy and cryotherapy
These can provide adequate treatment of early internal hemorrhoids. However, these therapies are infrequently used and generally reserved for grade I or II hemorrhoids. Although minimally invasive, they have a higher rate of post-procedure pain. Impotence, urinary retention, and abscess formation have also been reported. Recurrence rates are as high as 30%.
Laser therapy
Laser therapy is more costly and provides no advantage over other methods.
Surgical interventions
Surgical hemorrhoidectomy
Surgical hemorrhoidectomy is an effective treatment for all hemorrhoids indicated in the following situations:
About 5-10% of people with hemorrhoids eventually require surgical hemorrhoidectomy.
Postoperative pain remains the major complication, with most patients requiring 2-4 weeks before returning to normal activities. Other possible complications include urinary retention, anal stenosis and faecal incontinence.
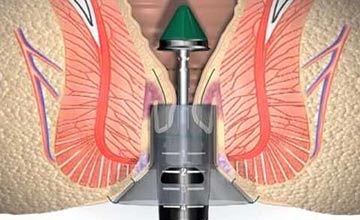
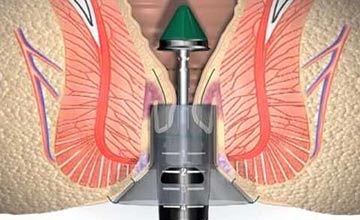
Doppler-guided trans-anal haemorrhoidal artery dearterialisation (THD) and rectoanal repair
Trans-anal haemorrhoidal dearterialisation (THD) and rectoanal repair (RAR) (THD with mucopexy) are minimally invasive alternatives to conventional hemorrhoidectomy that show promise for prolonged relief in patients with symptomatic hemorrhoidal disease. The advantages of transanal dearterialization include mild pain, fast recovery, low complication rate, and early return to daily activities.
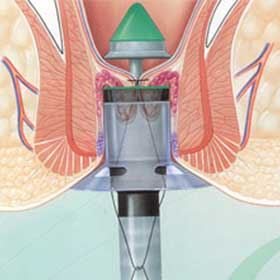
Stapled hemorrhoid surgery/procedure for prolapsing hemorrhoids (PPH)
Stapled hemorrhoid surgery, or PPH is suggested for patients with large internal hemorrhoids and minimal external component. During this procedure, a specially designed circular stapler is used to resect the excess tissue and lift the internal hemorrhoidal tissue left behind with interruption of the blood supply from above. Narcotic use and recovery is significantly decreased compared with conventional operative hemorrhoid surgery.
External Haemorrhoids
External haemorrhoids generally elicit symptoms due to acute thromboses (clots). Typically, acute thromboses spontaneously resolve in 10-14 days; therefore, a patient who presents late and has diminishing pain is best managed conservatively with pain-killers, cooling of the affected area and soothing baths.
Enucleation of the clot
This can be done under local anaesthetic in the outpatients if the patients present within 48-72 hours after the onset of pain. It has a significant recurrence rate approaching 30%.
Excision of the thrombosed haemorrhoid
This refers to the excision of the overlying skin and underlying veins, usually under a general anaesthetic. Suturing the wound closed is not necessary and may cause more pain.