 Wirral Surgeon
Excellence for Life
Wirral Surgeon
Excellence for Life
Condition treated
The most important point to remember is that everyone with a bowel problem can be helped and many can be completely cured.
It is never too late to get help with your bowel problems. If you would like some advice on how to approach your GP regarding your bowel problem do get in touch.

About Anal fistula
A fistula-in-ano is an abnormal hollow that connects a primary opening inside the anal canal to a secondary opening in the perianal skin; secondary tracts may be multiple and can extend from the same primary opening.
In the vast majority of cases, fistula-in-ano is caused by a previous anorectal abscess; formation of a fistula tract after anorectal abscess occurs in 7-40% of cases. Other fistulas develop secondary to trauma (eg, rectal foreign bodies), Crohn’s disease, anal fissures, anal carcinoma, radiation therapy, specific infections (actinomycoses, tuberculosis, chlamydia).
Clinical presentation
Signs and symptoms of fistula-in-ano, in order of prevalence, include the following:
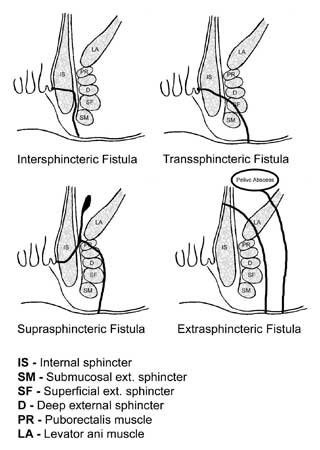
The relationship between the fistula tract and the anal sphincter is essential for treatment and prognosis. The Parks classification defines four types of fistula-in-ano that result from cryptoglandular infections, as follows:
Radiologic studies are not performed for routine fistula evaluation, because in most cases, the anatomy of a fistula-in-ano can be determined in the operating room. However, such studies can be helpful when the primary opening is difficult to identify or when recurrent or persistent disease is present. Endoanal or endorectal ultrasonography involves can help define the muscular anatomy and thereby help differentiate intersphincteric from transsphincteric lesions. Magnetic resonance imaging (MRI) is the study of choice for the evaluation of complex fistulas and recurrent fistulas. It has been shown to reduce recurrence rates by providing information on otherwise unknown extensions.
Management
Treatment of fistula-in-ano remains challenging. No definitive medical therapy is available for this condition, though long-term antibiotic prophylaxis and Infliximab may have a role in recurrent fistulas in patients with Crohn’s disease. Surgery is the treatment of choice, with the goals of draining infection, eradicating the fistulous tract, and avoiding persistent or recurrent disease while preserving anal sphincter function.
Surgery for fistula-in-ano should not be performed for definitive repair of the fistula in the setting of anorectal abscess. In the acute phase, simple incision and drainage of the abscess are sufficient; only 7-40% of patients will develop a fistula.
Fistulotomy (the laying-open technique)
It is useful for 85-95% of primary fistulas (ie, submucosal, intersphincteric, and low transsphincteric).
Beyond giving a visual identification of the amount of sphincter muscle involved, the purposes of setons are to drain, to promote fibrosis, and to cut through the fistula.
Mucosal advancement flap
Is indicated for the same disease process as seton use. Advantages include a one-stage procedure with no additional sphincter damage. A disadvantage is poor success in patients with Crohn disease or acute infection.
Fibrin glue and fistula plugs (Surgisis)
Lead to decreased postoperative morbidity and risk of incontinence, but long-term data are lacking for eradication of disease, especially in complex fistulas, which carry high recurrence rates.
Ligation of the intersphincteric fistula tract (LIFT)
It is a sphincter-sparing procedure for complex transsphincteric fistulas performed with the goal of performing a secure closure of the internal opening and by removing the infected cryptoglandular tissue.