Procedures
The most important point to remember is that everyone with a bowel problem can be helped and many can be completely cured.
Whenever possible, we offer procedures using minimally invasive techniques.
About Colonoscopy
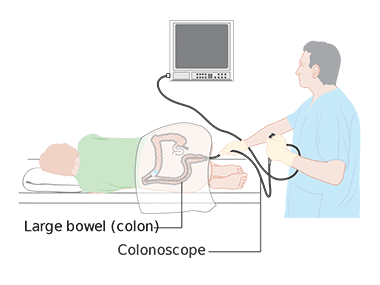
A colonoscopy is a procedure that uses a long, narrow, flexible, telescopic camera called a colonoscope to look at the lining of the large bowel (colon and rectum).
A colonoscopy can be used to detect irritated and swollen tissue, ulcers, or growths such as polyps. It helps to diagnose health conditions like Crohn’s disease, ulcerative colitis, diverticular disease and bowel cancer.
Indications
Colonoscopy is done to:
In addition to this, colonoscopy is often used to treat certain conditions:
Preparation
Patients need to have an empty bowel for the test in order for the colonoscopist to be able to clearly see the inside of the large bowel. Medications (laxatives) are prescribed the day before or/and the day of the test, depending on the slot allocated. In addition, diagnostic views are often improved if patients eat a low fibre diet for 1 or 2 days before the test. It is very important to drink plenty of clear fluids.
This includes:
After taking the laxatives you might need the toilet often and very suddenly. You may have some cramps. It is sensible to stay at home for a few hours after taking laxatives so that you are near a toilet. Patients who take iron tablets or other medicines that can cause constipation might need to stop taking these for 1 week before the test. Those who take medicines to thin the blood or are diabetic receive specific instructions depending on their underlying condition and specific medication taken.
During the procedure
The colonoscopy lasts approximately 20-60 minutes. Patients receive medication to make them feel relaxed and are asked to lie on your left side on the examining table. A rectal examination is usually performed just before the start of the procedure.
The colonoscopy is done with a colonoscope, a long, flexible, tubular instrument about ½ inch in diameter that transmits an image of the lining of the colon so it can be examined for any abnormalities. The colonoscope is inserted through the rectum and advanced to the other end of the large intestine, then slowly withdrawn while the lining of the bowel is carefully examined. The scope bends, so it can move around the curves of the large bowel; it also blows air into the colon, which expands the colon and allows a thorough inspection of its lining. Patients may be asked to change position occasionally to help advance the scope.
One may feel mild cramping during the procedure. This can be reduced by taking several slow, deep breaths during the procedure.
During the colonoscopy, if something is identified that may be abnormal, small amounts of tissue can be removed for analysis (called a biopsy) and abnormal growths, or polyps, can be identified and removed. In many cases, colonoscopy allows accurate diagnosis and treatment without the need for a major operation.
After the procedure
Patients usually stay in a recovery room for about 30 minutes for observation.
Some cramping or a sensation of having wind can be felt, but this usually passes quickly.
One will need to have a responsible adult to help with transport to home and overall supervision, as it is unsafe to drive, perform complex tasks, sign legally-binding documents or operate machinery for about 24 hours after the procedure (due to the sedative medication given).
Normal diet can be resumed almost immediately.
Certain medications, such as blood-thinning agents, may need to be avoided temporarily if biopsies were taken or polyps were removed.
Complications
Colonoscopy is a safe procedure, and complications are rare (around 2 significant complications in 1000 colonoscopies) but can occur:
Warning about colonoscopy
Bleeding and puncture of the colon are rare but possible complications of colonoscopy. Call the hospital or clinic immediately, or seek urgent medical advice if you have:
