Procedures
The most important point to remember is that everyone with a bowel problem can be helped and many can be completely cured.
Whenever possible, we offer procedures using minimally invasive techniques.
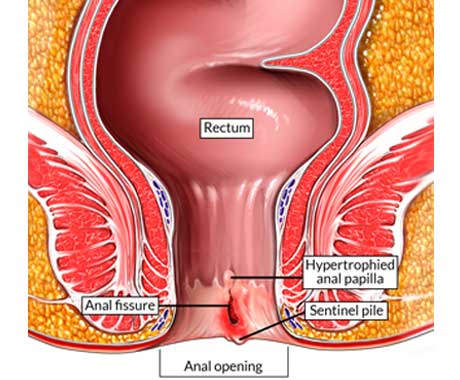
Anal Fissure
An anal fissure is a common and painful condition where a tear or ulcer develops in the anal canal, that's between the rectum and anal opening.
Pain from an anal fissure is usually felt when going to the toilet to pass a bowel motion, with a burning pain lasting for some hours afterwards.
Although many people feel embarrassed about talking to a doctor about symptoms of an anal fissure, it is important to get advice on relieving symptoms, as well as ruling out other causes of the symptoms, such as piles (haemorrhoids).
It is estimated that 1 in 10 people will experience an anal fissure during their life.
Surgical therapy is usually reserved for acute anal fissures that remain symptomatic after 4-6 weeks of medical therapy and for chronic anal fissures.
Preparation for surgery
The administration of an enema on the morning of the procedure is sufficient bowel preparation for surgical treatment of an anal fissure. If the fissure is too painful, the enema may be omitted.
Botox injection
Botulinum toxin (BOTOX®) can be used to treat acute and chronic anal fissures. It is injected directly into the internal anal sphincter, in effect performing a chemical sphincterotomy. The effect lasts about 3 months, until nerve endings regenerate. This 3-month period may allow acute fissures (and sometimes chronic fissures) to heal and symptoms to resolve. Success rates are in the region of 50%.
Lateral Internal Sphincterotomy
Lateral internal sphincterotomy is the current surgical procedure of choice for anal fissure. The procedure can be performed with the patient under general or spinal anesthesia. When treating a chronic anal fissure, the surgeon may elect to perform a fissurectomy in conjunction with the lateral sphincterotomy.
Advancement Mucosal Flap
Sometimes, long-standing chronic fissures do not heal, even with an adequate sphincterotomy, and an advancement flap must be performed to cover the defect in the mucosa. This can be performed either at the time of the sphincterotomy if the surgeon does not think that the fissure will heal, or as a second procedure if the fissure does not heal.
Postoperative recovery
Pain from the fissure starts to abate almost immediately. The only postoperative restrictions are from the anesthetic, and many patients can return to normal activities the following day.
Complications
Complications from surgery for anal fissure include the following:
Infection after sphincterotomy is rare and occurs as a small abscess in only 1-2% of patients, despite the inherent uncleanliness of the area. Treatment is drainage of the abscess. Antibiotics are necessary only if significant associated cellulitis occurs or if the patient is immunosuppressed.
Some ecchymosis (bruising) may occur around the sphincterotomy site, but bleeding that requires therapy is extremely rare.
Less than 1% of patients develop an anal fistula at the site of the sphincterotomy. This usually results from a breach of the mucosa at the time of the sphincterotomy. The fistula is often low and superficial and can be treated with fistulotomy.
The incidence and definition of incontinence vary dramatically from study to study. In most patients, the minor soiling or incontinence to flatulence that may occur in the immediate postoperative period usually resolves without any long-term sequelae.
