Wirral Surgeon - Surgical treatments is need and is divided into two categories: abdominal procedures and perineal procedures. The choice between an abdominal procedure and a perineal procedure is mainly dictated by the patient’s age and comorbidities.
Procedures
The most important point to remember is that everyone with a bowel problem can be helped and many can be completely cured.
Whenever possible, we offer procedures using minimally invasive techniques.
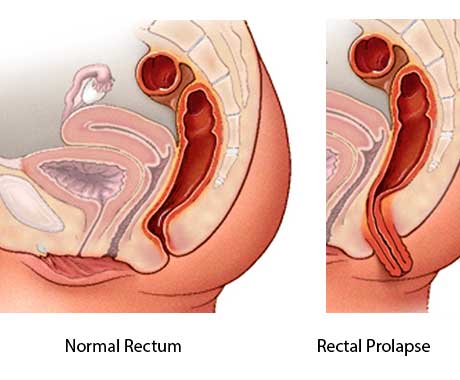
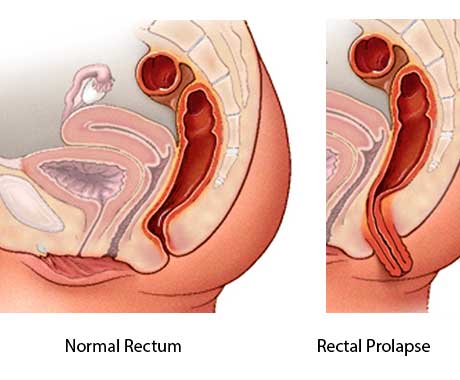
Rectal Prolapse Surgery
Surgical treatments can be divided into two categories according to the approach used to repair the rectal prolapse: abdominal procedures and perineal procedures. The choice between an abdominal procedure and a perineal procedure is mainly dictated by the patient’s age and comorbidities.
Rectal Prolapse Surgery
Surgical treatments can be divided into two categories according to the approach used to repair the rectal prolapse: abdominal procedures and perineal procedures. The choice between an abdominal procedure and a perineal procedure is mainly dictated by the patient’s age and comorbidities.
Perineal Procedures
These are easy to perform and have a good safety profile but have the disadvantage of a higher recurrence rate. For this reason, perineal procedures are generally recommended in older, frail patients, in whom a general anaesthetic and a prolonged operation might be contraindicated.
Anal encirclement (Thiersch wire)
With anal encirclement (Thiersch wire), a non-absorbable band is placed under the skin around the anus. Anal encirclement is usually reserved for only the most debilitated patients in whom palliation is the goal. Complications from this procedure include obstruction with fecal impaction and erosion of the wire with infection; it also carries a very high risk of fecal impaction.
Delorme mucosal sleeve resection
In a Delorme mucosal sleeve resection the lining is stripped from the rectum and excised; the prolapsed muscle is then pleated with a suture and reefed up like an accordion, and the transected edges of the mucosa are sutured together. This procedure is often used for small prolapses.
Altemeier perineal rectosigmoidectomy
In an Altemeier perineal rectosigmoidectomy, a full-thickness segment of bowel is transected and hand-sewn to the distal anal canal. This operation is relatively safe and effective in frail, older patients, with postoperative morbidity being low. However, the recurrence rate after the procedure is not negligible, and the operation is unpredictable in terms of restoring faecal continence.
Abdominal procedures
Abdominal procedures have a lower recurrence rate but are technically more demanding and require a general anaesthetic. Currently, most of these procedures are performed laparoscopically or robotically, with very good cosmetic results and early recovery.
Anterior resection
In an anterior resection for rectal prolapse the redundant colon (sigmoid) is resected and the left colon is anastomosed to the top of the rectum. At present, few colorectal surgeons perform this procedure, because it is not thought to address anatomic abnormalities such as poor rectal fixation.
Marlex rectopexy
In a Marlex rectopexy a non-absorbable material (mesh) is fixed to the sacrum and partially wrapped around the rectum to keep it in position. This procedure is associated with high rates of post-operative constipation and is therefore rarely performed currently.
Suture rectopexy
A suture rectopexy is essentially the same as a Marlex rectopexy, except that the rectum is fixed with suture material rather than mesh. Recurrence rates are higher and constipation might also be problematic.
Resection rectopexy
A resection with rectopexy (Frykman-Goldberg procedure) is a combination of an anterior resection and a Marlex rectopexy; it is a good option for patients with a significant component of constipation. It has the disadvantage of creating an anastomosis with risk of leakage.
Ventral mesh rectopexy
This is currently the gold standard in the treatment of rectal prolapse. It is associated with low rates of recurrence and post-operative constipation, and can treat other abnormalities of the pelvic floor at the same time.
Postoperative Care
Patients generally do well postoperatively, with minimal pain and a short hospital stay. Oral fluids and diet are commenced immediately after surgery. Bowel function returns quickly and patients can often be discharged 24-72 hours after the procedure.
Laxatives are generally prescribed for 2 weeks after discharge. There is no need for prolonged administration of antibiotics.
Skin sutures are absorbable and do not need to be removed.
Complications
Serious complications after rectal prolapse surgery are rare but include: