Wirral Surgeon - Colorectal cancer is the third most common cancer in the UK in both males and females and account for 12% of all diagnosed cancers. More than 40,000 cases of bowel cancer are diagnosed in the UK every year.
Condition treated
The most important point to remember is that everyone with a bowel problem can be helped and many can be completely cured.
It is never too late to get help with your bowel problems. If you would like some advice on how to approach your GP regarding your bowel problem do get in touch.
About Bowel Cancer
Colorectal cancer is the third most common cancer in the UK in both males and females and account for 12% of all diagnosed cancers. More than 40,000 cases of bowel cancer are diagnosed in the UK every year. One in 14 men and 1 in 19 women will be diagnosed with bowel cancer during their lifetime.
Bowel cancer is the second most common cause of cancer death in the UK, accounting for 10% of all cancer deaths (2014).
About Bowel Cancer
Colorectal cancer is the third most common cancer in the UK in both males and females and account for 12% of all diagnosed cancers. More than 40,000 cases of bowel cancer are diagnosed in the UK every year. One in 14 men and 1 in 19 women will be diagnosed with bowel cancer during their lifetime.
Bowel cancer is the second most common cause of cancer death in the UK, accounting for 10% of all cancer deaths (2014).
Risk factors
A person’s risk of developing cancer depends on many factors, including age, genetics, and exposure to risk factors (including some potentially avoidable lifestyle factors).
Occurrence of colorectal cancer is strongly related to age, with almost three‑quarters of cases occurring in people aged 65 or over.
Most people who develop bowel cancer have no family history of bowel cancer. However, for around 25% of all bowel cancer cases diagnosed in the UK there is a family history. Generally speaking, the more members of the family affected by bowel cancer and the younger they were at diagnosis, the greater the chance of a family link.
An estimated 54% of bowel cancers in the UK are linked to lifestyle factors including red and processed meat consumption (21%), overweight and obesity (13%), alcohol (12%), smoking (8%) and ionising radiation (2%).
Fibre consumption and physical activity protect against bowel cancer (inadequate levels are linked to an estimated 12% and 3% respectively of bowel cancer cases in the UK).
Asbestos exposure and certain medical conditions (inflammatory bowel disease, uretero-sigmoidostomy, pelvic radiation) and infections (Streptococcus bovis) may relate to higher bowel cancer risk.
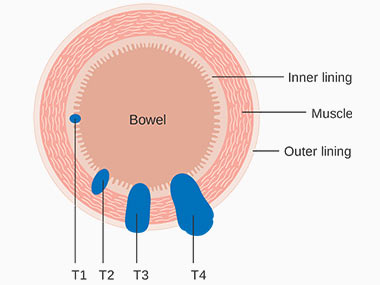
Survival
Around half of people diagnosed with colorectal cancer survive for at least 5 years after diagnosis. Survival is closely related to stage at diagnosis: the earlier the stage the greater the survival period. Patients with stage I disease have a 5-year survival rate in excess of 90%, whereas only 10% of patients diagnosed with stage IV colorectal cancer are still alive after 5 years.
Symptoms
In general symptoms of bowel cancer are very non-specific and overlap with those related to other diseases of the gastro-intestinal tract. In early stages bowel cancer can produce no symptoms. Weight loss is a generally a late symptom of bowel cancer and usually signals the presence of metastatic disease. Symptoms most commonly associated with bowel cancer include:
Diagnosis
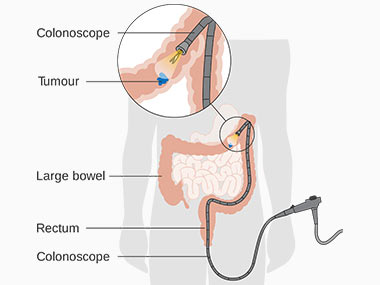
Colonoscopy
Optical colonoscopy remains the criterion standard against which the accuracy of other screening or diagnostic tests is measured. A major advantage of colonoscopy is that polyps can be excised during the procedure and samples can be taken for histopathological examination. However, it has a relatively higher cost and requires conscious sedation. Not all patients may be able to tolerate sedation, or it may be too risky to discontinue anticoagulation in persons with heart valves, for example.
CT Colonography
CT colonography, better known as virtual colonoscopy, is gaining in acceptance as an alternative or complementary diagnostic test to conventional colonoscopy. A common indication is for “completion colonography” following an incomplete optical colonoscopy. It is similar to diagnostic colonoscopy in that it requires 24 hours of bowel preparation with a combination of cathartics, contact laxatives, dietary restriction, and hydration. However, new developments in fecal tagging are able to eliminate the bowel preparation process.
Workup
Laboratory studies
These are done with a goal of assessing patients’ organ function (liver, kidneys) in anticipation of diagnostic and therapeutic procedures and also to estimate tumor burden. Studies may include the following:
A baseline CEA level should be obtained preoperatively as it carries prognostic value and when highly elevated may indicate more advanced, disseminated disease.
Imaging studies
Imaging is useful to stage the tumour in relation to local extent and distant metastatic spread and guide treatment modalities and combinations.
Computed tomography (CT) of chest/abdomen/pelvis. CT scanning can help identify the tumor site, the size of the tumor, and locoregional and metastatic spread, which can help guide surgical planning.
Magnetic resonance imaging (MRI) of pelvis/liver. MRI has roles in staging of rectal tumors and in assessment of liver metastases in colorectal carcinoma. Preoperative MRI is used to identify tumor distance from the mesorectal fascia, which is a predictor of tumor positivity at the circumferential resection margin (CRM) after a total mesorectal excision. MRI has been advocated as the most sensitive liver imaging in patients with colorectal cancer with liver metastases, who need evaluation for suitability for partial hepatectomy. MRI may also be used in symptom-based evaluations of other organs systems, if, for example, there is concern for brain metastasis or to characterize an adrenal mass in the setting of a patient with newly diagnosed colon carcinoma.
Positron emission tomography (PET) scanning is emerging as a very useful modality for staging and assessment of colorectal cancers. The newest addition, a fusion PET-CT scan, allows for detection of metastatic deposits and has the added tissue-based resolution of CT. Of note, some histologies, especially a mucinous signet-ring cell variant of colorectal cancer, may not be well visualized on a PET scan.
Ultrasonography (US). Transrectal ultrasound (TRUS) may be used to distinguish between layers of the rectal wall and thus detect depth of tumor penetration and perirectal spread.
Treatment
Surgery
Surgery is the only curative modality for localized colon and rectal cancer (stage I-III) and potentially provides the only curative option for patients with limited metastatic disease in liver and/or lung (stage IV disease). The general principles for all operations include removal of the primary tumor with adequate margins including areas of lymphatic drainage. Standard operations for adenocarcinoma of the colon and rectum are described in the 'Patient Information' section of the site.
Chemotherapy
Chemotherapy rather than surgery has been the standard management for patients with metastatic colorectal cancer. Biologic agents have assumed a major role in the treatment of metastatic cases, with selection increasingly guided by genetic analysis of the tumor. The proper use of elective colon/rectal resections in non-obstructed patients with stage IV disease is a source of continuing debate.
Adjuvant chemotherapy is standard for patients with stage III disease. Its use in stage II disease is controversial, with ongoing studies seeking to confirm which markers might identify patients who would benefit.
Radiotherapy
At present, the role of radiation therapy for colon cancer is limited to palliative therapy for selected metastatic sites such as bone or brain metastases.
Biologic agents
Biologic agents used in the treatment of colon and rectal cancer include monoclonal antibodies against vascular endothelial growth factor (VEGF) and epidermal growth factor receptor (EGFR), as well as a kinase inhibitor and a decoy receptor for VEGF. Such agents include the following:
These are useful therapeutic adjuncts in cases of metastatic colorectal cancer.